Research
What we do
The research of the Ferrall-Fairbanks BEAT Cancer Lab focuses on leveraging tumor heterogeneity to design personalized treatment schedules for cancer patients. Ecology and evolutionary forces of cancer allows a tumor to alter its growth and metastasis. Therefore, in close collaboration with clinicians and other cancer researchers, the BEAT Cancer Lab uses a mechanistic understanding of tumor composition to design innovative treatment schedules to control cancer growth and metastasis without compromising the health of the patient’s other organ systems.
How we do it
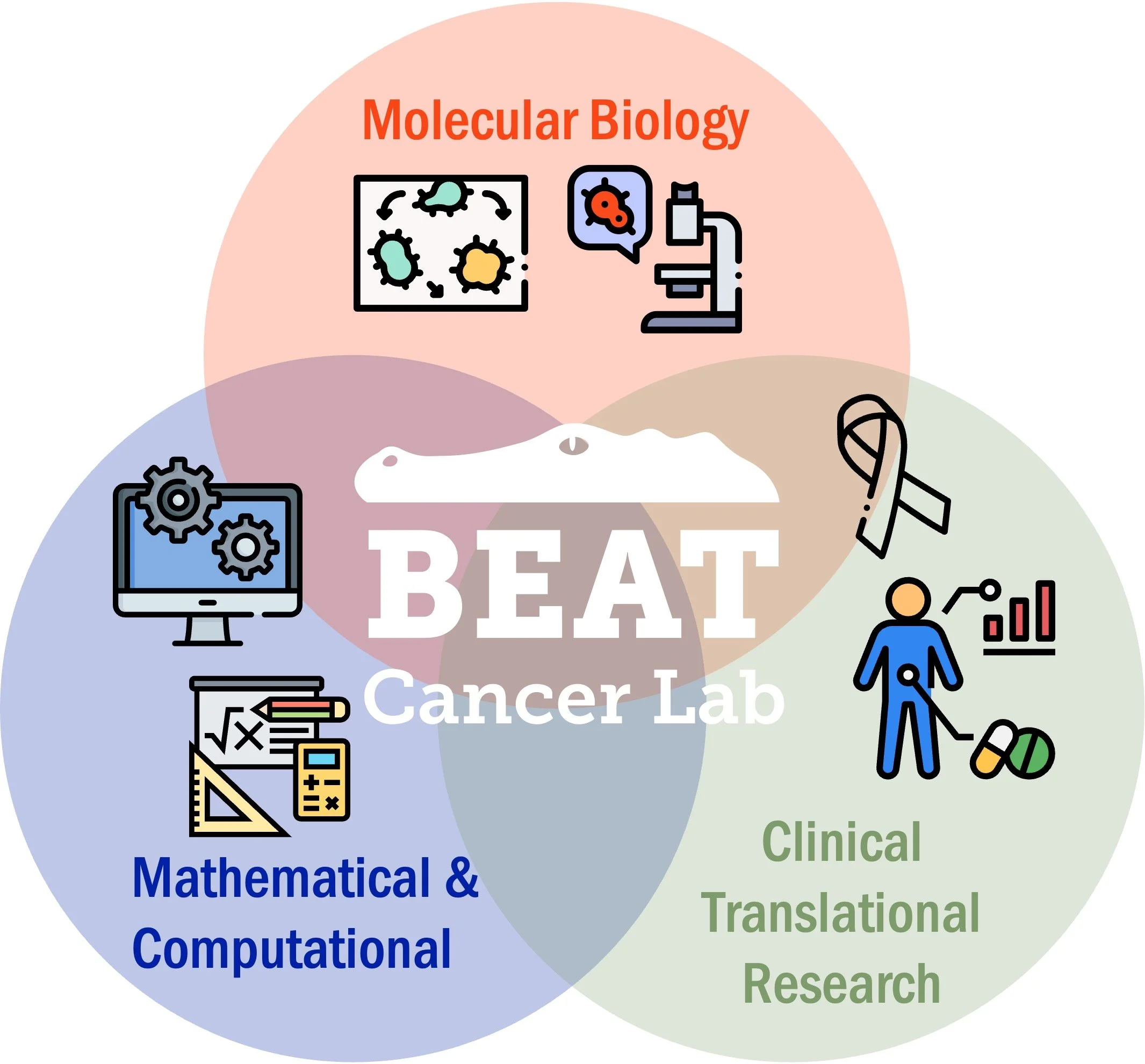
This requires multidisciplinary and team-science approaches to analyze and uncover the mechanisms driving cancer growth and evolution. The BEAT Cancer Lab integrates computational, mathematical, and wet-lab experimental techniques to investigate this heterogeneity at the molecular, tissue, and systems levels. Our overall aim is to exploit the eco-evolutionary dynamics of a tumor to develop treatment schedules to control cancer growth and minimize side effects. This supports the group’s long-term goal of bringing personalized, precision medicine to cancer patients.
Our Projects
Determine impacts of tumor composition & host environment on treatment response
Ovarian cancer is the most lethal gynecologic cancer in the world with over 80% of patients relapsing after first-round therapies and 1 in 6 dying within the first 3 months of diagnosis. We are applying evolutionary medicine approaches to better understanding of platinum-resistance for control of tumor growth. This project will generate computational models integrating data from clinical, molecular, and cellular scales to predict strategies for controlling ovarian cancer growth based on differences in tumor ecology and platinum-resistant populations. We will achieve this goal by (1) a retrospective study of the association of co-morbidities with platinum-sensitivity from patient records and (2) assessing the effects of different host environments by isolating the supporting stroma cells in ovarian tumors for co-culture with previously established platinum-sensitive and platinum-resistant ovarian cancer cells.
In collaboration with Dr. David Iglesias (UF) and Dr. Shelley Tworoger (Oregon Health and Science University)
Funded NCATS KL2 TROO1429
Integrative approaches to understand systems-level effects of chemotherapeutics
Cancer survivors in 18 of the top 20 site-specific cancers have elevated risks of cardiovascular events including venous thromboembolism, heart failure, arrhythmias, coronary artery disease, stroke, and valvular heart disease. As a result, cardio-oncology is a rapidly emerging field in medicine, focused on understanding the effects of cancer and cancer treatment on the heart. However, there are gaps in our knowledge about how these dysfunctions change the tissues’ biomechanical and biomolecular properties that can be assessed through an integrative approach. In this project, we are marrying the use of mathematical modeling and tissue-engineered cardiac platforms to assess changes in the biomolecular and biomechanical properties of the tissue in response to chemotherapeutic agents.
Determine targetable mechanisms of the evolution of inhibitor persistence
In this project, we are exploring the development mechanisms of PARP inhibitor persistence in ovarian cancer. Using in vitro models, different cellular constructs with different phenotypic features had PARP inhibitor persistence evolved to have pairs of sensitive and persistence cell lines with the same backbone. Each pair was then subjected to droplet-based single-cell RNA sequencing to explore the transcriptomic and metabolic changes that arose due to evolution of persistence with an aim at identifying potential therapeutic targets to disrupt the onset of inhibitor persistence/resistance.
In collaboration with Dr. Mehdi Damaghi (Stony Brook Cancer Center)
Exploring role of inflammatory insults on the leukemic self-renewing compartments
We seek to understand the relationship between inflammatory insults and its impact on the leukemic self-renewing compartment and ultimately disease progression of chronic myelomonocytic leukemia (CMML). To address this critical knowledge gap, we hypothesize that inflammation precipitates an adverse hematopoietic stem and progenitor cell (HSPC) state characterized by GMP expansion that represent a therapeutically exploitable, context specific evolutionary adaption. Using multi-omics approaches, we are characterizing the leukemic populations associated with adverse outcomes in CMML in a prospective clinical cohort.
In collaboration with Dr. Eric Padron (Moffitt Cancer Center), Dr. Mrinal Patnaik (Mayo Clinic), and Dr. Dana Rollinson (Moffitt Cancer Center)
Funded NCI R01 CA2783000
Determine associations between clinical outcomes and spatial heterogeneity metrics
We hypothesize that the spatial arrangement of different immune cells (or what we call their non-random immune distributions) can identify novel cellular relationships in the tumor-immune microenvironment (TIME) that correlate with clinical outcomes and are independent of commonly reported multiplex immunofluorescence metrics, such as cell density. In this project, we are testing this hypothesis in multiplexed images from kidney cancer samples from at least two distinct regions-of-interest per sample taken from the tumor, stroma, and interface between tumor and stroma. We are comparing the empirically found cellular marker distributions compared against the theoretical random probability density function and summarized using previously described distribution metrics and these values will be correlated with clinicopathologic outcomes.
In collaboration with Dr. Brandon Manley (Moffitt Cancer Center) and Dr. Philipp Altrock (Max Planck Institute)
Tools
We strive to develop transparent and reproducible workflows for both data analysis as well as mathematical models created by the BEAT Cancer Lab. In doing so, we make our code publicly available through GitHub and CodeOcean Capsules.